Nigeria: Cholera outbreak Cases of acute watery diarrhoea were first reported in April. An outbreak of cholera has now been confirmed with over 1,900 suspected cases, and more than 35 deaths, from Kwara, Zamfara and Lagos and most recently Borno State.
Cholera outbreaks occur frequently in the country. Treatment centres are being set up in affected areas Cholera It spreads via contaminated food and water include vomiting and profuse, watery diarrhoea which can lead to severe dehydration
Recommendations: Travellers staying in quality accommodation are at lower risk Consider vaccination Pay strict attention to hygiene drink only boiled or bottled water, water that has been treated with chlorine or iodine, or carbonated beverages. Select food, water and other beverages carefully. choose food that has been thoroughly cooked while fresh and is served hot. Avoid ice, raw fruit, and raw vegetables (including salad). Fruit and vegetables that you peel yourself are safer choices. Pay close attention to hygiene. Wash your hands frequently, especially before eating
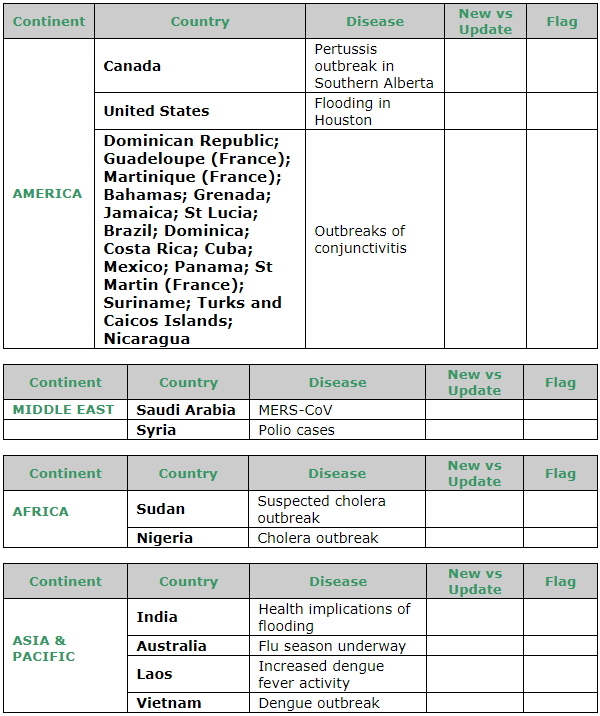
Syria: Polio cases At least 33 children who developed paralysis in Mayadeen district, Deir-Al-Zour, have been confirmed to be infected by circulating vaccine-derived poliovirus type 2 (cVDPV2). Additional cases in Deir-Al-Zour, Homs and Raqqa governorates are positive for cVDPV2. They all reported symptoms beginning between 3 March and 13 July. Several healthy contacts in the community have also tested positive. Surveillance has been stepped up and vaccination campaigns for children under 5 years have commenced in order to prevent the disease from spreading further Cases of wild polio virus have not been recorded in the country since 2013-2014
POLIO - Poliovirus only infects humans. It is very contagious and spreads through person-to-person contact. The virus lives in an infected person’s throat and intestines. It enters the body through the mouth and spreads through contact with the feces (poop) of an infected person and, though less common, through droplets from a sneeze or cough. You can get infected with poliovirus if you have feces on your hands and you touch your mouth. Also, you can get infected if you put in your mouth objects like toys that are contaminated with feces. : About 1 out of 4 people with poliovirus infection will have flu-like symptoms that may include: Sore throat / Fever / Tiredness / Nausea / Headache / Stomach pain These symptoms usually last 2 to 5 days then go away on their own. A smaller proportion of people with poliovirus infection will develop other more serious symptoms that affect the brain and spinal cord: * (feeling of pins and needles in the legs) * (infection of the covering of the spinal cord and/or brain) occurs in about 1 out of 25 people with poliovirus infection * (can’t move parts of the body) or weakness in the arms, legs, or both, occurs in about 1 out of 200 people with poliovirus infection Paralysis is the most severe symptom associated with polio because it can lead to permanent disability and death. Between 2 and 10 out of 100 people who have paralysis from poliovirus infection die because the virus affects the muscles that help them breathe
Recommendations: Ensure you are up to date with polio vaccination, including one booster as an adult. Select food, water and other beverages carefully. Drink only boiled or bottled water, or sealed carbonated beverages. Choose food that has been thoroughly cooked while fresh and is served hot. Avoid ice, raw fruit, and raw vegetables (including salad). Pay attention to hygiene. Wash your hands frequently, especially before eating
United States: Flooding in Houston Harvey – the biggest storm in the state's history – has caused many injuries, several fatalities, and widespread damage to property and infrastructure. Much of Houston is flooded and is expected to remain so for weeks. Essential services are interrupted. Transportation issues may delay the appropriate treatment of injuries and illnesses. Medical facilities may have reduced ability to treat patients. There is an increased risk of injury, and a risk of water and food-borne, mosquito-borne and other communicable diseases. All non-essential travel to Houston should be deferred. Those in affected areas should follow the directions of local authorities, avoid floodwaters and be careful in selection of water and food.
Americas: Outbreaks of conjunctivitis A surge in cases of conjunctivitis has been reported in several Central American countries and Caribbean islands. the Bahamas, Brazil, Costa Rica, Cuba, Dominica, the Dominican Republic, Grenada, Guadeloupe, Jamaica, Martinique, Mexico,
Nicaragua, Panama, Saint Lucia, Saint Martin, Suriname, and the Turks and Caicos Islands. Bahamas is experiencing a 28% increase in conjunctivitis cases as compared to the activity seen during the same period last year. Brazil has reported cases in Amazonas, Rondonia, Sao Paulo and Santa Catarina states. In Costa Rica, the canton of Garabito is most affected. Cases were recorded in towns of Herradura, Jacó Centro, Quebrada Ganado, Quebrada Amarilla and Tárcoles, At least seven health districts have been affected in Dominica. The Dominican Republic has reported around 155,000 conjunctivitis cases since May. A majority of the cases were reported from the provinces of Distrito Nacional, San Cristobal, Santiago and Santo Domingo. In Guadeloupe, a recent surge in case numbers is recorded to be about eight times higher than last year. Affected areas include Grand Bourg, Le Gosier, Pointe-a-Pitre and Terre-de-Bas. In Martinique, Marin and Francois are reported to be most affected. Martinique reports over 15,000 suspected conjunctivitis cases, mostly in the communes of Robert, Diamant and Lamentin. Many states of Mexico report that the increase in disease activity is much higher than that seen last year. Nicaragua has reported over 11,000 cases nationwide in 2017, with a large surge in cases since mid-August. The most affected departments are Chinandega, Leon, Managua, Rivas, and the Northern and Southern Caribbean Coasts. At least nine health regions in Panama have been affected including Colon Province. Saint Lucia and Saint Martin have reported an increase in cases in July. Over 1300 cases have been reported in Suriname from all of its ten districts Cuba has reported over 1400 cases, most from Guantanamo, followed by Santiago de Cuba, Havana, Ciego de Ávila and Tunas. Health authorities in the affected regions are implementing measures to control the spread of infection
Conjunctivitis - Viruses and bacteria can cause conjunctivitis which spread from one person to another are usually mild. Eyes become red or pink, itchy and watery
Recommendations: Viral conjunctivitis usually resolves on its own without treatment, while infection caused by bacteria is treated with antibiotic drops. Practice good hygiene. Avoid touching your eyes., and Wash your hands thoroughly and frequently. Do not touch your eyes. Do not share personal hygiene or grooming items such as washcloths or make-up
Laos: Increased Dengue fever activity Following a small outbreak earlier in the year, there has been an increased number of dengue cases reported since mid-April. Over 6,700 cases have been detected since the start of the year, including at least ten deaths Dengue Fever - Dengue is spread by mosquitoes High fever and at least two of the following: Severe headache / Severe eye pain (behind eyes) or joint pain / Muscle and/or bone pain / Rash / Low white cell count and Mild bleeding manifestation (e.g., nose or gum bleed, petechiae, or easy bruising) Watch for warning signs as temperature declines 3 to 7 days after symptoms began. seek medical help if any of the following warning signs appear: Severe abdominal pain or persistent vomiting / Red spots or patches on the skin / Bleeding from nose or gums / Vomiting blood / Black, tarry stools (feces, excrement) / Drowsiness or irritability / Pale, cold, or clammy skin / Difficulty breathing
Recommendations: Although a vaccine has been developed, it is only available in a small number of countries and is not recommended for travellers. Prevent infection by avoiding mosquito bites, When outdoors, wear clothing that covers most of your body (long sleeves, long pants, socks). Use an effective insect repellent that contains DEET, Picaridin, PMD, or IR3535. Ensure windows are covered with fly-wire. Use "knock-down" insect spray to kill mosquitoes in your room and choose air conditioned accommodation if possible. Seek medical attention if you develop a high fever, especially if you suffer "rigors" (shaking) or a rash
Vietnam: Dengue outbreak Dengue activity this year is significantly higher than usual. Over 90,000 cases and at least 24 fatalities have been reported since the start of the year. Although the majority of cases have occurred in the south, northern Vietnam is also experiencing a surge, with Hanoi particularly affected. The World Health Organization is supporting the Ministry of Health in their response. Measures to control mosquito breeding and hospital capacity to detect and treat the disease have been increased D
engue Fever - Dengue is spread by mosquitoes High fever and at least two of the following: Severe headache / Severe eye pain (behind eyes) or joint pain / Muscle and/or bone pain / Rash / Low white cell count and Mild bleeding manifestation (e.g., nose or gum bleed, petechiae, or easy bruising) Watch for warning signs as temperature declines 3 to 7 days after symptoms began. seek medical help if any of the following warning signs appear: Severe abdominal pain or persistent vomiting / Red spots or patches on the skin / Bleeding from nose or gums / Vomiting blood / Black, tarry stools (feces, excrement) / Drowsiness or irritability / Pale, cold, or clammy skin / Difficulty breathing
Recommendations: Although a vaccine has been developed, it is only available in a small number of countries and is not recommended for travellers. Prevent infection by avoiding mosquito bites, When outdoors, wear clothing that covers most of your body (long sleeves, long pants, socks). Use an effective insect repellent that contains DEET, Picaridin, PMD, or IR3535. Ensure windows are covered with fly-wire. Use "knock-down" insect spray to kill mosquitoes in your room and choose air conditioned accommodation if possible. Seek medical attention if you develop a high fever, especially if you suffer "rigors" (shaking) or a rash
Sudan: Suspected cholera outbreak Over 30,000 cases of acute watery diarrhoea, some confirmed as cholera have been reported in Sudan since August 2016. Every state has reported cases of acute watery diarrhoea (AWD) but significantly affected states include Blue Nile, Central Darfur, Gezira, Kassala, Khartoum, North Darfur, North Kurdufan, South Kurdufan, Kal-Qadarif, Red Sea, Sennar, South Darfar, West Darfur and White Nile. In August, AWD infections have extended into Northern State (ash-Shamaliyah) and more than 650 deaths have been linked to the outbreak. Cholera is consistently present in the country and outbreaks are also ongoing in the neighbouring countries of South Sudan and Ethiopia Cholera - It spreads via contaminated food and water include vomiting and profuse, watery diarrhoea which can lead to severe dehydration Recommendations: Travellers staying in quality accommodation are at lower risk Consider vaccination Pay strict attention to hygiene drink only boiled or bottled water, water that has been treated with chlorine or iodine, or carbonated beverages. Select food, water and other beverages carefully. choose food that has been thoroughly cooked while fresh and is served hot. Avoid ice, raw fruit, and raw vegetables (including salad). Fruit and vegetables that you peel yourself are safer choices. Pay close attention to hygiene. Wash your hands frequently, especially before eating
Canada: Pertussis outbreak in Southern Alberta An outbreak of pertussis (whooping cough) is ongoing in Southern Alberta.
Year of Diagnosis Zone South Calgary Central Edmonton North Total Count Count Count Count Count Count 2017 324* 37 134 97 47 639 Pertussis
Pertussis is a very contagious disease only found in humans. It is spread from person to person. People with pertussis usually spread the disease to another person by coughing or sneezing or when spending a lot of time near one another where you share breathing space. Many babies who get pertussis are infected by older siblings, parents, or caregivers who might not even know they have the disease. Infected people are most contagious up to about 2 weeks after the cough begins The disease usually starts with cold-like symptoms and maybe a mild cough or fever. In babies, the cough can be minimal or not even there. Babies may have a symptom known as "apnea." Apnea is a pause in the child's breathing pattern. Pertussis is most dangerous for babies. About half of babies younger than 1 year who get the disease need care in the hospital. Early symptoms can last for 1 to 2 weeks and usually include: Runny nose / Low-grade fever (generally minimal throughout the course of the disease) / Mild, occasional cough / Apnea – a pause in breathing (in babies) Because pertussis in its early stages appears to be nothing more than the common cold, it is often not suspected or diagnosed until the more severe symptoms appear
Late-stage Symptoms After 1 to 2 weeks and as the disease progresses, the traditional symptoms of pertussis may appear and include: Paroxysms (fits) of many, rapid coughs followed by a high-pitched "whoop" Vomiting (throwing up) during or after coughing fits Exhaustion (very tired) after coughing fits Pertussis can cause violent and rapid coughing, over and over, until the air is gone from the lungs and you are forced to inhale with a loud "whooping" sound. This extreme coughing can cause you to throw up and be very tired. Although you are often exhausted after a coughing fit, you usually appear fairly well in-between. Coughing fits generally become more common and bad as the illness continues, and can occur more often at night. The coughing fits can go on for up to 10 weeks or more. In China, pertussis is known as the "100 day cough." However, the "whoop" is often not there for people who have milder (less serious) disease. The infection is generally milder in teens and adults, especially those who have been vaccinated.
Recommendations: The best way to prevent pertussis (whooping cough) among babies, children, teens, and adults is to get vaccinated. Also, keep babies and other people at high risk for pertussis complications away from infected people.The recommended pertussis vaccine for babies and children is called DTaP. This is a combination vaccine that helps protect against three diseases: diphtheria, tetanus and pertussis To practice good hygiene you should: Cover your mouth and nose with a tissue when you cough or sneeze. Put your used tissue in the waste basket. Cough or sneeze into your upper sleeve or elbow, not your hands, if you don't have a tissue. Wash your hands often with soap and water for at least 20 seconds. Use an alcohol-based hand rub if soap and water are not available.
Australia: Flu season underway Flu season is underway affecting most states of Australia. Queensland, New South Wales and the Australian Capital Territory (ACT) are reporting earlier activity at higher rates than seen in previous years. The A(H3N2) strain is responsible for the majority of infections, although influenza B strains are also circulating. The current southern hemisphere influenza vaccine covers these strains Influenza / Flu - Flu is a viral illness, transmitted person be person via air droplets sudden fever, cough, headache, weakness and muscular pains. Most cases are mild although some can be severe or even fatal
Recommendations: consider using a mask. The pregnant women, adults over 65 and young children are at higher risk of severe illness. Prevention is through vaccination and attention to hygiene, ensure you have had your annual seasonal flu vaccine. pay close attention to hygiene and avoid people who are obviously sick
India: Health implications of flooding Maharashtra, Assam, Arunachal Pradesh, Bihar, Meghalaya, Orissa, Sikkim, Tripura, Uttar Pradesh, West Bengal - India Dengue fever, Diarrhoea, Hepatitis A, Leptospirosis, Cholera, Japanese encephalitis, Malaria, Typhoid fever, Influenza Many parts of Assam, Arunachal Pradesh, Bihar, Maharashtra, Meghalaya, Odisha (Orissa), Sikkim, Tripura, Uttar Pradesh and West Bengal states have been affected. Floods are known to occur most years during the monsoon season. Although no major outbreaks of infectious diseases have yet been reported, diarrhoea and potentially serious gastrointestinal illnesses (such as typhoid, hepatitis A and cholera) may occur. Wounds can become infected after contact with contaminated water and the risk of leptospirosis is higher. Mosquito-borne diseases may increase, including chikungunya, dengue fever, malaria and Japanese encephalitis. Displaced animals may carry rabies and be more prevalent in the environment than usual
Saudi Arabia: MERS-CoV In August 2017, over thirty cases of MERS-CoV were recorded. Affected places include Aldelem, Alaflaj, Beljershi Albaha, Dawmat Aljandal, Hail, Jeddah, Madinah and Najran. Both primary and secondary cases were recorded and some had underlying health problems. Contact tracing is underway. Some people who have tested positive for the virus have no symptoms, some have had a mild illness, while others are critically ill, and fatalities continue to be reported. Three unrelated clusters of MERS cases have been identified between April and June. One of the affected hospitals is located in Bisha city, Assir Region. The other two outbreaks are centred around hospitals in Riyadh and Wadi Aldwaser cities of Riyadh Region. Cases include healthcare workers, patients and household contacts of the ''index'' cases.
What is MERS-CoV- Middle East respiratory syndrome coronavirus (MERS-CoV), known previously as "novel coronavirus", was first identified in humans in 2012. It is from the same family of viruses as SARS (Severe Acute Respiratory Syndrome), the coronavirus family. Most cases have originated from the Middle East, although a large outbreak associated with hospitals occurred in South Korea in 2015. While some people may have no symptoms at all, others may have a fever and cough. Some, particularly those with underlying health issues, progress to a severe disease with pneumonia and respiratory failure. About 30-40% of cases are fatal. Outbreaks and clusters of infection have occurred in the healthcare environment and within household Spread can occur from one person to others in close contact, possibly through infected respiratory droplets
Recommendations: There is no specific treatment and no vaccine available. Avoid direct contact with dromedary camels, consuming undercooked camel meat, or drinking raw camel products (milk, urine etc)1